Brachial Plexus Injury Care
What Is the Brachial Plexus?
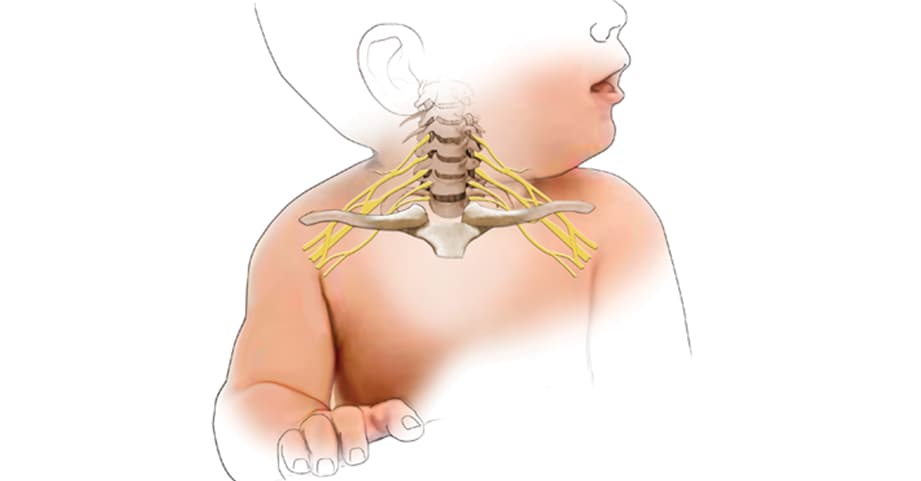
The brachial plexus is a group of nerves that exit the spinal cord at the base of the neck. These nerves carry signals to and from your brain and spine, and down your arm. They control movement and sensation for the shoulder, arm, elbow, wrist and hand—from the shoulder to the fingertips.
A New Brachial Plexus Clinic
Our multidisciplinary Brachial Plexus Clinic brings together orthopedic specialists, physiatrists, and physical and occupational therapists who are specially trained to treat kids with brachial plexus birth injury or brachial plexus birth palsy.
REQUEST AN APPOINTMENTBrachial plexus birth injury (BPBI) is trauma to an infant’s brachial plexus that happens during childbirth. It results in varying degrees of paralysis or loss of movement of the arm, shoulder, elbow, wrist, hand or fingers. If an infant's paralysis mainly involves the shoulder and often, it is often called Erb's palsy.
A child with BPBI will move one arm much less than the other. It is rare for both arms to be affected. It is can also be associated with other childbirth injuries like a clavicle or humerus fracture, and it can go unnoticed for two to three weeks after birth.
BPBI occurs in 1 to 3 in every 1,000 births.
What are symptoms of brachial plexus birth palsy?
Your baby may:- Have a single arm or hand that seems clearly weak.
- Have trouble controlling his arm or hand muscles.
When should I call a doctor?
You should call your child’s pediatrician or Children's Healthcare of Atlanta at 404-785-HAND (4263) if your child has:
- Seeming discomfort in the neck and shoulders.
- Weakness in the hands or arms.
- Pain or weakness in both arms.
What causes brachial plexus birth palsy?
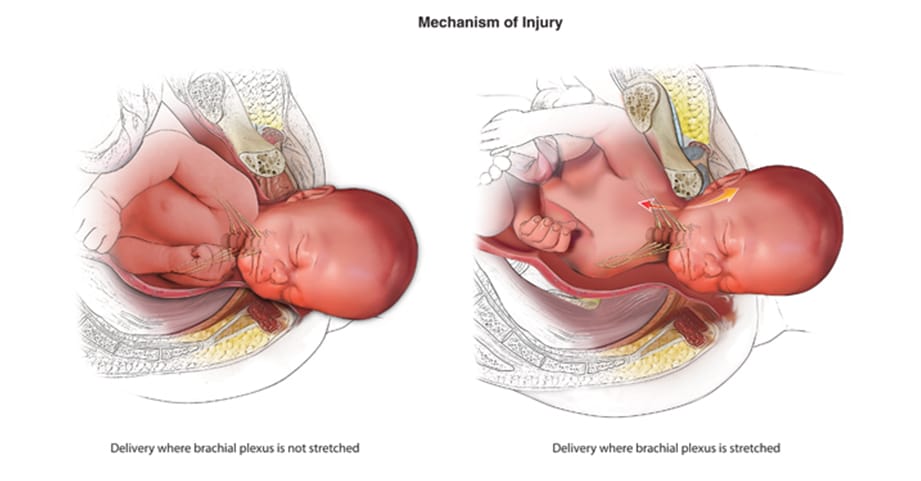
The most common causes are:- A difficult birth.
- A large baby as a result of gestational diabetes or a delivery past term.
- Mother’s history of children born with BPBI.
What is the prognosis if a child has brachial plexus birth injury?
Recovery depends on the type of injury and how many nerves are affected. Most children with BPBI can expect a full recovery without any therapy or surgery. It is important for a specialist to evaluate a child who may have BPBI to help watch the child’s progress and identify treatment options. It is best to begin treatment soon after birth in order to explore all treatment options, but we are often able to help a child at any age.
- Most children do not need surgery. If a child does not gain sufficient recovery by 3 to 6 months old, he or she may need surgery as an infant.
- Some children are left with a degree of paralysis and may benefit from reconstructive surgery as toddlers or adolescents.
Brachial plexus injuries, not related to birth, are uncommon but can be more significant. They can result from car accidents and significant falls. Minor brachial plexus injuries often occur during athletic activities and competitions. They are also known as burners or stingers.
What are symptoms of a brachial plexus injury?
Symptoms of a brachial plexus injury may include your child experiencing:- A feeling like an electric shock or a burning sensation shooting down his arm
- Loss of sensation or numbness
- Weakness or inability to use certain muscles in the hand, arm or shoulder
- Complete lack of movement or paralysis in the hand, arm or shoulder
- Severe pain
Early diagnosis of a brachial plexus injury is important because symptoms can be permanent if left untreated. It is important to see a doctor if your child or teen experiences any of the symptoms associated with a brachial plexus injury.
What causes a brachial plexus injury?
A brachial plexus injury may be caused by:- Sports injuries
- Car, motorcycle and boat accidents
- Falls
What are the types of brachial plexus injuries?
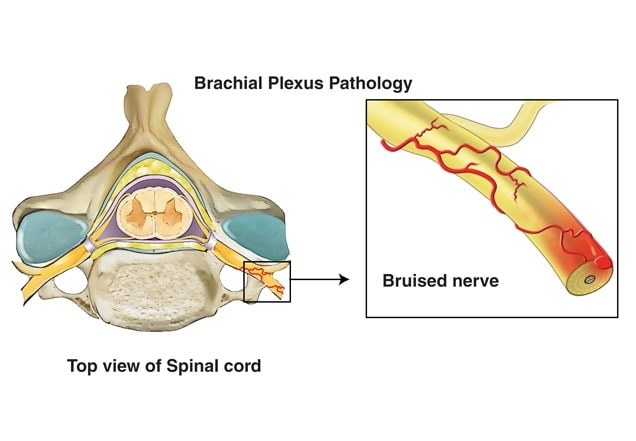
A brachial plexus injury damages some or all of these nerves. There are five common types of the injury:
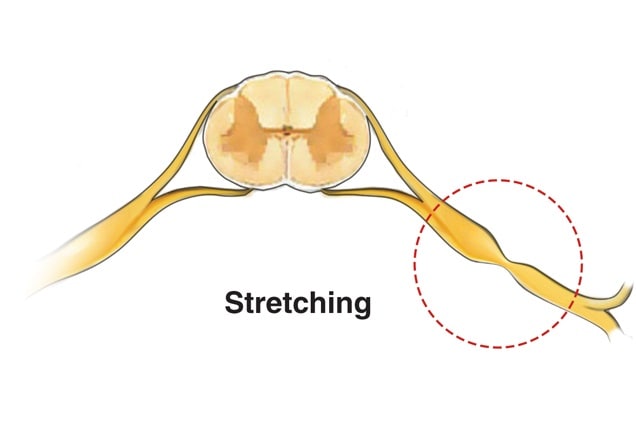
Stretching injuries result from stretching the nerves too far. For instance, when the head and neck are forced away from the shoulder, the nerves might be damaged.
This is how the nerves are injured during birth and in sport-related incidents. Sports-related incidents are often referred to as burners or stingers. Symptoms can last from a few minutes up to a few days. The nerves may heal on their own depending on how far they were stretched.
An avulsion happens when a nerve is stretched so far that it is actually pulled apart from the spinal cord. It is the most severe nerve injury and can only be treated with surgery.
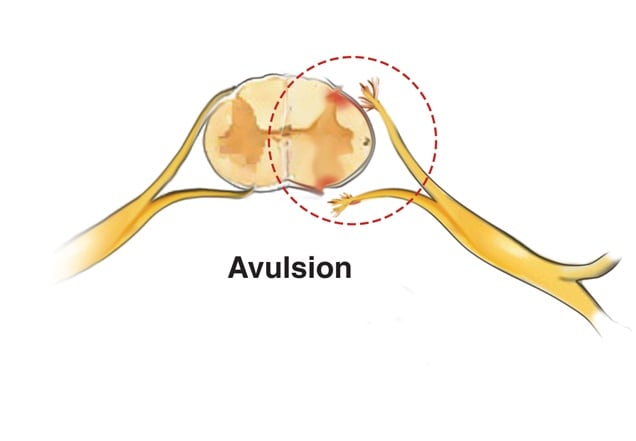
A rupture happens within the nerve itself when it is forcibly stretched far enough that the actual nerve is torn apart into more than one piece. Like avulsion, a rupture can result in a completely or partially paralyzed arm and can only be treated with surgery, such as nerve grafting or a nerve transfer.

A contusion is a bruise. The brachial plexus can be bruised when it is squeezed or crushed. A brachial plexus contusion can cause pain and numbness down the arm.
Penetrating injuries can result in cuts and tears in the brachial plexus. For instance, shards of glass from a car accident can cut the nerves. These injuries happen less often.
Before deciding on a treatment plan for your child’s brachial plexus injury, our team will evaluate your child’s condition. There are no simple tests to figure out exactly how severe the injury is or what nerves are damaged.
Your child’s evaluation may include:
- A complete medical history in which we will ask you questions about your child’s previous health conditions.
- A physical examination in which your child’s doctor will be looking for:
- How well your child’s muscles are developed.
- Whether your child uses muscles in the shoulder, arm and hand.
- Whether he has feeling in his arm.
- What your child can do with the uninjured arm compared to the affected arm.
Our goal is to improve your child’s arm strength and movement. Full recovery depends on early testing, education and treatment. While it is best to begin treatment right after birth or injury in order to keep all options available, but we are often able to help a child at any age or time from injury.
It is difficult to tell soon after a brachial plexus injury whether it will result in permanent damage. The severity of the injury will likely determine your child’s treatment and outcome. The earlier a brachial plexus injury is treated, the better the chances for full recovery.
Our services
We provide coordinated, comprehensive care for infants, children and teens with acute and chronic brachial plexus injuries, including brachial plexus birth palsy and other palsies. Our treatment includes:
- Multispecialty physician evaluation
- Reconstructive nerve surgery
- Soft tissue and bone reconstructive surgery
- Occupational therapy
- Physical therapy
- Splint fabrication
- Family education, including home therapy teaching, like foreign language translation
For patients that need an X-ray, our radiologists use low-dose protocols to limit the amount of radiation each patient receives. Our pediatric anesthesiologists are trained to provide the most appropriate dose of sedation for patients that need surgery.
In addition, Children’s has the only hospital-based pediatric orthotics and prosthetics lab in Georgia. For patients who have limited mobility in their arms, shoulders, elbows, wrists, hands and fingers after treatment, we offer rehabilitation through our Hand and Upper Extremity Therapy Program.

If your child is under 18, he should see a pediatric orthopedic specialist.
A child’s musculoskeletal system is different than an adult, so it’s important your child be treated by a team that specializes in treating children—from birth to 18—for orthopedic conditions.
Learn moreIf your child has been diagnosed with BPBI or a brachial plexus injury, he may need to participate in physical, occupational or hand therapy to help treat the condition.
Brachial plexus birth injury
Before the age of 2, treatment is geared toward maintaining mobile joints. Physical therapy and home exercise programs are an important part of keeping the joints moving so they do not get stiff. During this time, we watch for progress and look for problems like painless shoulder dislocation. If examinations and tests show that the shoulder is dislocated, surgery will be needed. If your child’s shoulder is not dislocated but is becoming increasingly tight, surgery may be needed to loosen the joint to prevent deformities later in childhood.
By age 2, a child has likely reached the limit of his natural recovery. At this point, a blend of therapy and surgery may help.
Brachial plexus injuries
Early treatment for a brachial plexus injury often involves physical, occupational or hand therapy at home and in a physical therapy clinic. At first, therapy will focus on maintaining your child’s joint motion. Our team will also work with him to build his range of movement and strength. Family members are encouraged to get involved. We will educate your child and family about which exercises to do at home and how to do them.
Surgery may be needed if your child has been diagnosed with BPBI or brachial plexus injury, depending on his age, the length of time since the injury, and how well your child can move and function. Our pediatric hand and upper extremity surgeons will work with you to determine if surgery is best for your child. Nerve surgeries are usually only successful when performed within a few months of the injury, which is why early treatment is beneficial. After a period of time, such as a year from injury, nerve surgeries can be ineffective.
Surgery performed soon after a BPBI or brachial plexus injury may include:
Nerve repair and grafting
During this procedure, a pediatric surgeon repairs the brachial plexus or removes the damaged portion of one or more of the nerves and replaces it with a healthy nerve.
Nerve transfer
This procedure involves the pediatric surgeon connecting part of a nerve with a different purpose to a nerve that is not working in order to restore movement and feeling. Connecting a working nerve, or part of a working nerve, to the nerve that is not working helps restore lost movement. The “donor” nerve is usually a redundant branch so that there is no loss of major function once it is transferred to restore lost function.
There are numerous types of nerve transfer options. Your pediatric surgeon will help determine which one is best for your child.
Surgery for BPBI and Brachial Plexus Injuries Long After Surgery
Surgery for toddlers, school-age children and teens may include:
Tendon transfer
During this procedure, a pediatric surgeon moves a healthy muscle or tendon to the damaged area in order to help improve functions that are lost or weakened by an injury. For example, the muscle that allows your child to bring his arm to his body can be moved to allow him to lift his arms above his head or to his side. As with nerve transfers, the muscle selected to restore function is typically redundant and will not result in major loss of function.
Osteotomy
The pediatric surgeon cuts the bone and moves it to correct or improve the position. In some children, the forearm becomes contracted in a way that a child cannot turn his palms up or down. A similar surgery can be done on the forearm to help improve position and function.
Free muscle transfer
This procedure involves a pediatric surgeon transplanting an entire muscle, along with its nerve and blood vessels, from another part of the body into the arm. The transferred muscle, usually a less important leg muscle, is controlled by a living nerve and revived by local blood vessels.
Bone and joint surgeries
These surgeries are used to reposition joints to enhance function. They are often used to treat the later effects of nerve injuries.
U.S. News & World Report ranks us among the top pediatric orthopedics programs in the country. Our program combines the latest proven technology and research with a caring, child-friendly approach, making Children's a top choice for treatment of orthopedic conditions and injuries.
Our doctors and surgeons work closely with pediatric surgeons in the community to help so that complete, coordinated care may be delivered seamlessly at our hospitals for children with orthopedic conditions. Our Brachial Plexus Program is led by Medical Director Allan E. Peljovich, MD, MPH. You can reach the Brachial Plexus Program team at brachialplexusclinic@choa.org or 404-785-HAND.
Children's Physician Group
Physiatry
Community providers
Hand surgeons
Center for Advanced Pediatrics
2174 North Druid Hills Road NE
Atlanta, GA 30329
This content is general information and is not specific medical advice. Always consult with a doctor or healthcare provider if you have any questions or concerns about the health of a child. In case of an urgent concern or emergency, call 911 or go to the nearest emergency department right away. Some physicians and affiliated healthcare professionals on the Children’s Healthcare of Atlanta team are independent providers and are not our employees.
Contact Us 404-785-HAND (4263)
















