Legg-Calve-Perthes Disease
Two major components of the hip joint are the femoral head (ball-shaped head of the thighbone) and the acetabulum (socket). Legg-Calve-Perthes disease, commonly referred to simply as Perthes disease, is a childhood hip condition in which the femoral head loses its blood supply and collapses. When this happens, a part of or all of the area involved temporarily dies. It is important to understand that the socket is not affected or involved in this loss of blood supply. The body will absorb the dead bone cells and replace them with new bone cells. The new bone cells eventually reshape the femoral head of the thighbone. Legg-Calve-Perthes disease causes the hip joint to become painful and stiff. It can also leave the femoral head deformed and lead to disability.
The cause of Perthes disease is unknown, but we do know that it:
- Is four times more likely in boys than girls.
- Commonly affects firstborn children.
- Is most often seen in children 4 to 8 years old, but it can affect children 2 years old to teenagers.
- Affects only one hip in most cases. It can involve both, but it does not happen to both at the same stage.
- Has not been proven to be inherited.
Perthes disease goes through four phases:
- Phase 1: Blood stops reaching the femoral head, and the hip joint becomes inflamed, stiff and painful. Portions of the bone turn into dead tissue. The ball of the thighbone becomes less round. This phase can last from several months up to one year.
- Phase 2: The body cleans up the dead bone cells and replaces them with new, healthier bone cells. The femoral head begins to remodel into a round shape again. The joint is still irritated and painful. This phase can last one to three years.
- Phase 3: The femoral head continues to model itself back into a round shape with new bone. This phase lasts one to three years.
- Phase 4: Normal bone cells replace new bone cells. This last phase can last a few years to complete the healing process.
It is important to understand that every affected child goes through each phase, from beginning to end. This whole process can extend over many months to years.
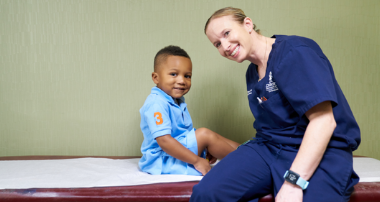
Legg-Calve-Perthes disease: Identifying Joseph’s rare condition
After hip and knee pain kept Joseph Morris from walking comfortably, the Children’s orthopedic team identified his rare condition as Legg-Calve-Perthes disease.
Read his storyThe most common signs of Perthes disease include:
- Walking with a slow limp that occurs at irregular intervals.
- Having limited range of motion in the hip.
- Having pain in the hip, thigh or knee, though pain is not usually a major factor. Pain often seems more activity-related.
These symptoms may resemble other hip conditions or medical problems, so it’s important to talk to your child’s doctor. Due to the slow onset and minimal pain, it may be months before parents seek help. Often, children will complain of knee pain, even though the problem is located in the hip. During the initial examination, the doctor may find a child that limps has loss of motion around the hip and, in cases of longer duration, evidence of muscle wasting.
Our pediatric orthopedics team at Children’s takes a specialized approach to diagnosing Perthes disease in children and teens. This may include:
- Complete medical history and physical examination
- X-ray
- CT scan
- MRI
- Arthrograms, a dye injected into the hip to determine the shape and status of the femoral head
- Blood tests
- Bone scans
Our team of pediatric orthopedic specialists will work with you to create a treatment plan for your child’s Legg-Calve-Perthes diagnosis based on:
- Age, overall health and medical history
- Amount of hip pain or stiffness
- Degree of femoral head collapse
- Progression of the condition
- Tolerance for certain medications, procedures or therapies
- How the condition is likely to affect your child
- Your opinion or preference
The goal of treating Perthes disease is to preserve the roundness of the femoral head and prevent deformity while the condition runs its course. At first, treatment focuses on regaining hip motion and reducing pain from the tight muscles around the hip and inflammation inside the joint. Maintenance of good hip motion and containment (keeping the ball in the socket) is important. The socket (not involved in Perthes disease) acts as a template to help shape the deformed femoral head during healing.
A long-term study identified four major factors that impact the outcome of recommended treatments for Perthes disease:
- The child’s age at onset, which is probably the most important factor influencing the outcome.
- Children under 6 often have good long-term outcomes regardless of the treatment.
- Children 6 to 8 years old have the most varied treatment options and outcomes.
- Children 8 and older are often recommended to have surgery.
- The extent of involvement of the femoral head (the percent losing its blood supply). If the area is small, the outcomes are better.
- The ability to keep the femoral head in the acetabulum during the disease process, also called containment.
- Loss of motion of the hip joint.
Our team doesn’t have control over the first two factors outlined above, so we focus on the last two outcomes during management or treatment of Perthes disease.
Treatment may include:
- Bed rest and traction.
- Casting or bracing to hold the femoral head in the hip socket, restrict joint movement and allow the femur to remold itself into a round shape again. A brace may be used to maintain containment. Plaster casts are often used temporarily while the brace is being manufactured.
- Crutches or a wheelchair.
- Medications, such as ibuprofen, to help with inflammation.
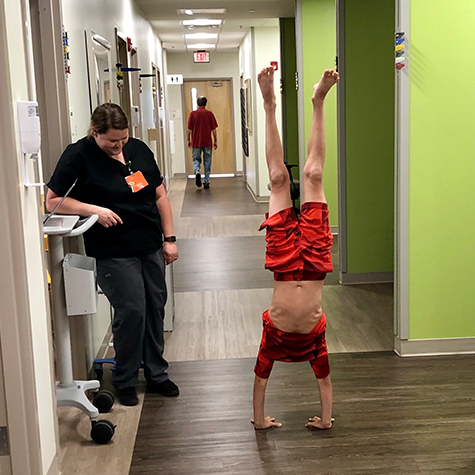
- Physical therapy to keep the hip muscles strong and to promote hip movement.
- Reduced activity.
- Routine examinations performed by your child’s doctor to help ensure progress.
- Surgery to better position the femoral head in the hip socket (femoral osteotomy) or to increase blood flow to the femoral head (core decompression).
Studies show that up to 90% of patients are active and pain-free 30 to 40 years after disease onset. This means that while most hips will not return to normal shape, your child will enjoy the ability to keep up with friends as they go through life.
Support on Facebook
Contact Us 404-255-1933