Cell and Gene Therapy Research
The Cell and Gene Therapy Program at the Aflac Cancer and Blood Disorders Center of Children’s Healthcare of Atlanta has three major initiatives focused on the engineering of cellular products to treat childhood cancer:
- Development of drug-resistant immunocompetent cells for brain cancer
- Generation of anti-neuroblastoma cellular therapeutics
- Creation of chimeric antigen receptor technologies (CAR-T) for T-cell leukemia
Although we continue to advance our Cell and Gene Therapy Program toward clinical applications, we are also dedicated to building the personnel and infrastructure necessary to apply these technologies in Phase 1 clinical trials. Our main focus is to obtain U.S. Food and Drug Administration (FDA) approval as quickly as possible. Initiating gene-based trials is a complex process that requires the involvement of clinical and research faculty, technical expertise, and regulatory personnel, who are available through various programs within the Aflac Cancer and Blood Disorders Center.
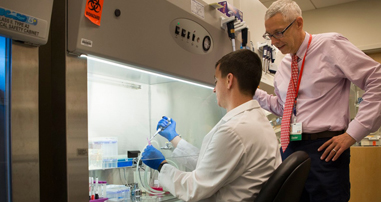
A scientific team at the Aflac Cancer and Blood Disorders Center, led by Christopher Doering, PhD, Assistant Professor of Pediatrics at Emory University School of Medicine, and H. Trent Spencer, PhD, Assistant Professor of Pediatrics at Emory University and Director of the Cell and Gene Therapy Program at the Aflac Cancer and Blood Disorders Center, has discovered how to engineer CAR-T cells to kill cancer by using the immune system of a lamprey, a prehistoric fish.
There is considerable academic and industrial interest in developing CAR-T variants, which can attack brain cancer, neuroblastoma, sarcoma and other cancers that afflict children. The substantial challenge is to achieve the selective killing of cancer while minimizing any collateral damage to normal tissue.
Drs. Spencer and Doering worked with Max Cooper, MD, Professor of Pathology and Laboratory Medicine at Emory University, to generate data showing that it is feasible to engineer human cells to express lamprey-derived variable lymphocyte receptors (VLR) as part of an entirely new CAR-T concept. In short, this is a highly disruptive lab breakthrough that may allow for productive development of CAR-T to treat cancer broadly in children and adults.
Our goal is to treat children with incurable cancer. The pathway involves focused lab work by Aflac Cancer and Blood Disorders Center scientists requiring an FDA license as well as a pharmaceutical-grade facility on-site that will allow for the manufacturing of VLR T-cells and related technologies for use in children with cancer and catastrophic diseases.
The Emory Personalized Immunotherapy Center (EPIC) is leading trials involving the manufacturing and delivery of stem cell therapies for patients with leukemia who are undergoing blood and marrow transplant (BMT) procedures. Scholars from EPIC are working in collaboration with the Aflac Cancer and Blood Disorders Center team toward a breakthrough in cell immunotherapy for pediatric cancer with VLR T-cells.
Led by Benjamin K. Watkins, MD, and Muna Qayed, MD, researchers at the Aflac Cancer and Blood Disorders Center published findings that the risk for acute graft-versus-host (GVHD) disease dropped to 3% with the addition of the drug abatacept.
Read moreCarlton Dampier, MD, Professor and Assistant Dean for Clinical Research at Emory University, along with an international team of pain experts, received funding from a five-year National Institutes of Health (NIH) R01 grant for the iCanCope With Sickle Cell Disease Program, which is being developed for children with sickle cell disease who experience frequent pain.
The program consists of personalized goal setting to improve pain and function, pain self-management training and rehearsal, and peer-based social support through a supervised, closed online community for children and young adults with sickle cell disease. These components are delivered on the iCanCope smartphone app and are complemented by sickle cell disease self-management education on the iCanCope website. The website education component includes specific modules designed to empower parents and caregivers to promote disease self-management in their children.
The program will be developed and tested by the Sickle Cell Program at the Aflac Cancer and Blood Disorders Center, Connecticut Children’s Medical Center, and the Hospital for Sick Children in Toronto, Canada. The grant began in September 2016 and runs through August 2022 and provides $2.02 million in funding.
Drs. Doering and Spencer co-authored an article that was published in Nature, a weekly international scientific journal, online databases and services across the life, physical, chemical and applied sciences, as well as clinical medicine.
The article, “Enhancing the Pharmaceutical Properties of Protein Drugs by Ancestral Sequence Reconstruction,” was the result of tests and studies conducted by the research team. It is about how the optimization of a protein’s pharmaceutical properties is usually carried out by rational design and/or directed evolution. The team tested an alternative approach based on ancestral sequence reconstruction. Using available genomic sequence data on coagulation factor VIII and predictive models of molecular evolution, the team engineered protein variants with improved activity, stability and biosynthesis potential and reduced inhibition by anti-drug antibodies. In principle, this approach can be applied to any protein drug based on a conserved gene sequence.