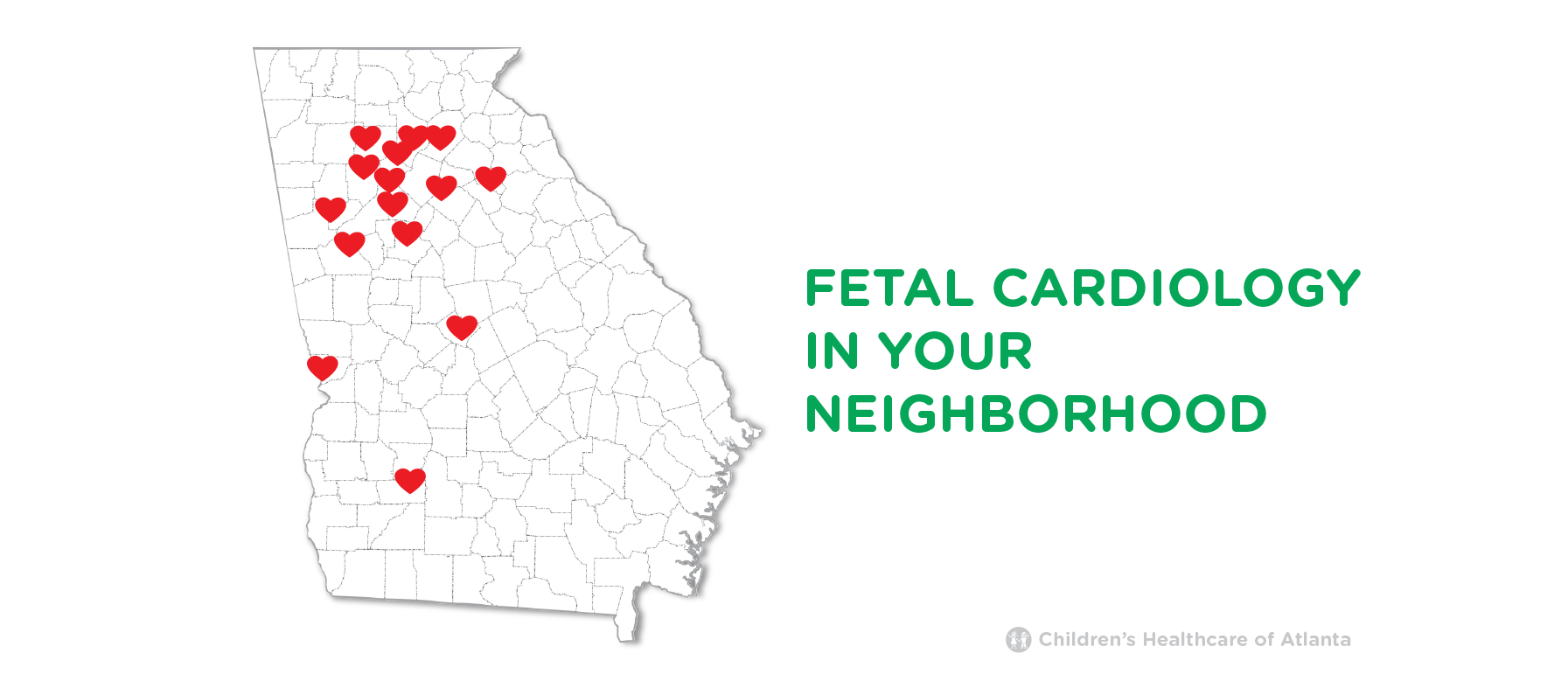
The Fetal Cardiology Program at the Children’s Healthcare of Atlanta Heart Center provides specialized care to diagnose fetal heart conditions before a baby is born, consults mothers whose unborn children have suspected or known heart problems, and delivers treatment to help babies born with heart conditions live healthy lives. One of the largest programs of its kind in the country, the Fetal Cardiology Program at the Children's Heart Center has more than 20 highly skilled fetal cardiologists on staff to accurately diagnose congenital heart defects, also known as congenital heart disease, or CHD's. We provide each family with a comprehensive fetal heart evaluation, consultation that offers detailed future care recommendations for the referring physician and family, as well as post-natal management of the newborn. While most parents are referred to the Children's Heart Center, we offer locations throughout Georgia where a parent can receive a fetal cardiac evaluation, providing convenient access to high-quality fetal heart care.
Who needs to see a fetal cardiologist?
You may be referred to a fetal cardiologist if:
- An ultrasound or anatomy scan shows a possible heart condition in the fetus.
- The mother, father or siblings of the unborn baby have a history of heart problems.
- The fetal heartbeat is abnormal or irregular, or if a heart murmur is identified.
- A genetic or chromosomal condition is identified in the fetus.
- Abnormalities in the unborn baby's other major organ systems, such as the brain, kidneys or lungs, are identified by ultrasound.
- The mother has a medical condition, such as diabetes or phenylketonuria (PKU), or a connective tissue disease, such as lupus or Sjogren's syndrome that can affect the unborn baby's heart.
- The mother has been exposed to viruses, or certain medicines or drugs that can affect development of the unborn baby's heart.
Our Fetal Cardiology Program collaborates with local and regional obstetricians, maternal-fetal medicine specialists, neonatologists and delivery centers as an extension of their care, and if a fetal heart problem or congenital heart defect is diagnosed, provides seamless access to pediatric cardiologists, cardiothoracic surgeons and cardiac intensivists who develop family-centered treatment plans based on the unique needs of the unborn baby and family. We offer a variety of resources including prenatal genetic counseling, social work support and access to specialized cardiac nurses.
To learn more about our Fetal Cardiology Program, contact Kendall Haney, Clinical Nurse Coordinator, at 404-785-8745.
Heart defects and conditions we diagnose and treat include:
- Atrioventricular (AV) canal defect
- Coarctation of the aorta
- Fetal arrhythmia
- Atrial flutter
- Supraventricular tachycardia (SVT)
- Heart block
- Fetal heart failure
- Hypoplastic left heart syndrome (HLHS)
- Single ventricle heart disease
- Tetralogy of fallot
- Transposition of the great arteries (TGA)
- Ventricular septal defect

Questions to ask during a fetal echocardiogram
A fetal echocardiogram is an imaging test that allows a doctor to observe the structure of an unborn baby’s heart for any potential heart conditions. Learn what to ask the doctor about your baby's heart during this test.
read moreCaring for the Tiniest Hearts
-
Children's Fetal Cardiology Program
The Fetal Cardiology Program at the Children’s Heart Center delivers care to expectant mothers whose unborn children have suspected or known heart defects.
- Coordinated Care: We offer a team-based approach to care that includes collaboration and high-risk delivery planning with OB and maternal-fetal medicine delivery centers.
- Experience: The fetal cardiologists at Children's are extensively experienced and performed over 3,000 fetal echocardiograms in 2024.
- Accreditation in Fetal Echocardiography: The Fetal Cardiology Program at Children’s received the Intersocietal Accreditation Commission (IAC), a distinction that recognizes facilities that provide outstanding echocardiogram study completeness, image quality and accuracy.
The Children’s Heart Center is ranked as one of the best pediatric cardiology and heart surgery programs in the country by U.S. News & World Report* with some of the highest volumes in the country for heart surgeries, catheterizations and heart transplants. Our Fetal Cardiology Program is one of the largest of its kind in the country, and you can rest assured knowing that we treat all kinds of heart problems every day to help children live healthy lives.
Leading the Way in Innovating and Advancing Pediatric Heart Care
Fetal Echocardiogram
A fetal echocardiogram, also known as a fetal echo or fetal echocardiography, is a highly sensitive ultrasound test that provides high-quality, accurate images of an unborn baby's heart. Typically, doctors will perform this test to assess the fetal cardiovascular system when a fetus is at 18-24 weeks, often in relation to the mother's 20-week ultrasound. However, due to significant advances in ultrasound technology that allows visualization of very small cardiac structures, this test may be done earlier in the pregnancy—as soon as 13-14 weeks gestation. A fetal echo takes approximately 40 to 60 minutes to complete, depending on the complexity of the heart problem.
The results of this test provide doctors with information about the heart anatomy and function that allows them to counsel families with pregnancies complicated by a fetal cardiac abnormality.
A fetal echocardiogram will:
- Check your baby’s heart structure, rhythm and function.
- Help the medical provider identify and monitor a heart problem.
- Check to make sure your baby is growing and developing well.
Early Pregnancy Fetal Cardiac Imaging
Our Fetal Cardiology Program has the expertise to assess the fetal heart as early as 13-14 weeks gestation. Early testing, such as maternal blood screening for fetal DNA or nuchal translucency screening, can identify pregnancies at risk for chromosomal anomalies and/ or structural heart disease very early in the pregnancy. Echocardiography helps confirm a diagnosis, so families can know as early as possible if their baby has a cardiac abnormality.
Situations in which early gestation fetal cardiac imaging may be recommended include:
- A suspected genetic or chromosomal condition.
- A history of a prior pregnancy affected by a CHD.
- A first-degree relative with a CHD.
- Because early fetal cardiac echocardiography is a new technology, we recommend in most cases that mothers have a repeat study at 18-20 weeks into the pregnancy to confirm the initial findings.
We can provide families with reliable diagnoses of fetal cardiac abnormality in those high-risk pregnancies where early diagnosis is desired. Because early fetal cardiac imaging is a novel technology, we do recommend in most cases that mothers undergoing early fetal echocardiography have a repeat study at 18-20 weeks gestation to confirm the initial findings.
If testing shows your unborn baby has a heart defect, we will work with the maternal-fetal medicine specialist, a high-risk obstetrician, to develop a follow-up schedule for monitoring. We will help you understand your baby's condition and needs so that you can make informed decisions for your family.
If your baby's heart condition requires surgery after delivery, we can help prepare you ahead of time by connecting you with a pediatric cardiothoracic surgeon and providing helpful resources.
Learning that your unborn baby has a heart defect can be scary and difficult to comprehend. We have collaborated with other institutions and the Pediatric Congenital Heart Association to create a printable guided questions tool so that you know the right questions to ask your physician.
Prenatal Simulation
The Children’s Heart Center offers a Simulation program designed to prepare you for your baby’s care after heart surgery. It is available for expectant parents who have a baby that will need heart surgery in the first month after birth.
Our simulation program is led by a nurse who will use a medically realistic doll with the type of tubes and equipment you will see on your baby after heart surgery. The nurse will show you each tube and piece of equipment, and you will listen to a recording of Cardiac Intensive Care Unit (CICU) sounds to help you know what to expect. You will have a chance to practice holding the medical doll so it will feel familiar when you hold your baby in the CICU. You will learn the roles of your care team and have a chance to ask questions.
We offer a second simulation for after your baby’s recovery in the CICU when they are ready to be transferred to the Cardiac Acute Care Unit (CACU). The simulation nurse will help you learn about the tubes and equipment your baby will have in the CACU, as well as the care needed to go home from the hospital. You will learn the roles of the care team in the CACU and have the opportunity to ask any questions you may have.
Simulations are held at Arthur M. Blank Hospital and are typically offered during a regular visit to the Fetal Cardiology Program.
Each simulation will take about 45 minutes.
Please let the Fetal Cardiology Nurse Coordinator know you would like to participate. The nurse coordinator will arrange for you to meet with the simulation nurse when you come back for one of your fetal cardiology visits.
Our team will work closely with your obstetrician and maternal-fetal medicine specialist to determine the best delivery plan for your baby. If a certain hospital location or mode of delivery is indicated, we will work with you and your family to help this process go as smoothly as possible. Based on your prenatal imaging, our fetal cardiologists will make recommendations regarding the timing of cardiology evaluation and care of the baby's heart condition after delivery. This recommendation is communicated to your obstetrician, specialist and delivery center.
If your baby has heart surgery after they are born, we will care for them in the Children’s Cardiac Intensive Care Unit (CICU) after surgery. We have one of the largest dedicated CICUs in the country with 48 total beds and an experienced staff who strives to deliver the highest quality care for your baby. Once your baby is medically stable, they will be moved from the CICU to the Cardiac Acute Care Unit (CACU), where they will receive care from specially trained cardiac nurses and cardiologists.
Parents are strongly encouraged to stay overnight in their child’s CACU room. During this time, you can provide emotional support to your child while also receiving the education and training you need to safely care for your child at home. If there are times when you can’t stay with your child, parents can call the CACU to speak with their child’s nurse and get a medical update.
Prior to your child’s discharge, their needs, such as nutrition, respiratory care, physical therapy and medication therapy, are carefully assessed. A plan for addressing these needs will be created by the attending physician with input from the Children's interdisciplinary team, which includes a registered nurse, social workers, case managers, therapists, dietitians, child life specialists and other caregivers. We will make sure you have access to educational materials, teaching tools and phone numbers to call if you have questions or concerns about your child's health.
Before your child goes home, parents are required to attend the following classes:
- CPR class
- Car seat class (if your child is a newborn)
- Cardiac surgery discharge class
All classes are free for parents and caregivers. We require that at least one parent take each class if your child has had heart surgery. The car seat class is required if your child is a newborn and has never been home. You must bring your child's car seat and base for inspection.
Our Fetal Cardiology Program team, as well as the Children’s Heart Center team of cardiologists, cardiothoracic surgeons and genetic counselors who support the program, are dedicated to the health and well-being of children born with a heart defect.
- Erik Michelfelder, MD, Director
- Kendall Haney, BSN, RN, Clinical Nurse Coordinator
- Laura Lei Castillo, BSN, RN, CPN, Clinical Nurse
Cardiologists
- Wesley Blackwood, MD
- William Border, MD
- Brian Cardis, MD
- Andrew Dodgen, MD
- Matthew Ferguson, MD
- Brandon Harden, MD
- Glen Iannucci, MD
- P. Andrea Kropf, MD
- Clifford Wesley Lindsey, MD
- William Mahle, MD
- William McEachern, MD
- Rachel McKay, MD
- Andrew Porter, MD
- Sanghee Suh Ro, MD
- Ritu Sachdeva, MD
- Denver Sallee, MD
- Divya Suthar, MD
- Benjamin Toole, MD
- Neill Videlefsky, MD
- Michelle Wallace, MD
Cardiothoracic surgeons

Arthur M. Blank Hospital
With the opening of Arthur M. Blank Hospital, clinical services at Egleston Hospital, the Emory Children’s Center and the Aflac Cancer and Blood Disorders Center moved to the new hospital.
learn more*No. 12 on the U.S. News & World Report “Best Children’s Hospitals” list for 2024-25.
Contact Us 404-256-2593